Posted in Cardiopulmonary Bypass | 14/01/2015
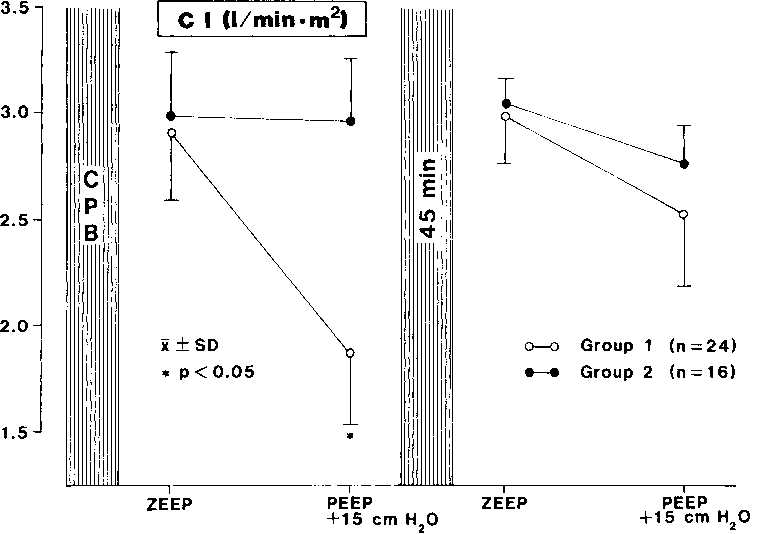
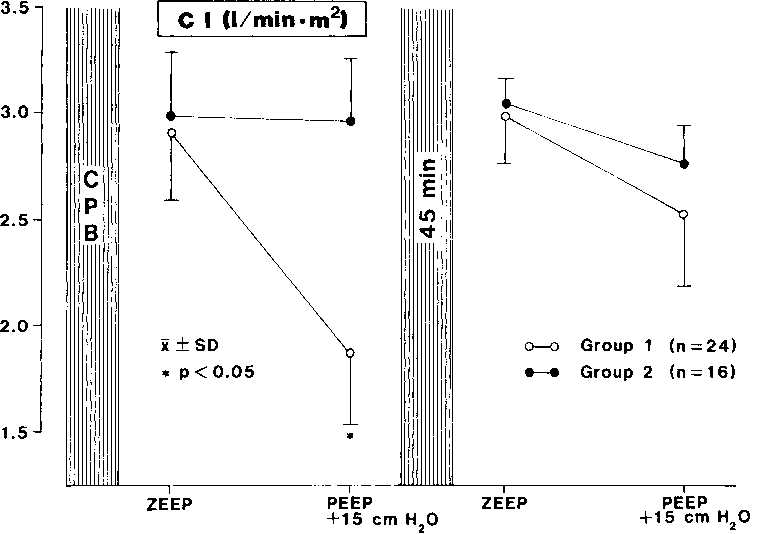
The patients were retrospectively subdivided into two groups according to the change in RVEF after PEEP application immediately after weaning from CPB: group 1 (n = 24), where RVEF decreased, and group 2 (n = 16), where RVEF remained almost unchanged. Using analysis of co-variance, the degree of RCA-stenosis was detected to be the decisive factor for the change in RVEF. Analysis of preoperative catheterization data revealed that in patients in group 1, stenosis of the right coronary artery (RCA) was significantly more pronounced (with RCA-stenosis) in comparison to patients in group 2 (without RCA-stenosis). Only in patients of group 1, RCA revascularization or coronary end-arterectomy (CEA) was performed. The biometric data were without differences between the groups (Table 2).
Read more
Posted in Cardiopulmonary Bypass | 13/01/2015
The multilumen balloon-flotation pulmonary artery catheter used in this study was specially designed to measure right ventricular ejection fraction (RVEF). It is mounted with a fast response thermistor (FRT), which is rapid enough to record beat-by-beat the plateaus of the rapid step changes on the descending limb of the thermodilution washout curve. This technology allows determination of the residual end-diastolic blood volume (RVEDV) with the help of a bedside microprocessor (REF-1, Edwards Lab, Santa Ana, CA); RVESV (RVEDV-stroke volume) and RVEF (EDV-ESV/EDV) were calculated, too. Theoretic background and detailed technical features have been discussed elsewhere. CO and RVEF were measured in triplicate at the end of the expiration and its mean values were used for statistical analysis.
Read more
Posted in Cardiopulmonary Bypass | 12/01/2015
Controlled mechanical ventilation with positive end-expiratory pressure (PEEP) is ubiquitously used in patients with pulmonary failure, although its beneficial influence on the respiratory system is accompanied by detrimental effects on the circulatory system. The mechanism by which PEEP ventilation decreases cardiac output (CO) has been the subject of several investigations, but it still is not entirely clear. The decrease in CO is attributed mainly to a decrease in venous return due to elevated intrathoracic pressure. Other studies suggest that this effect is caused by an increase in right ventricular afterload due to an increase in pulmonary impedance, decreased biventricular end-diastolic volume, altered ventricular interdependence by leftward displacement of the ventricular septum, or decreased myocardial contractility due to altered myocardial blood flow or a myocardial depressing factor induced by PEEP The use of PEEP after cardiopulmonary bypass (CPB) seems reasonable, but its routine application is controversially discussed because of its possible…
Read more
Posted in Bronchus Avulsion | 11/01/2015
Most tracheobronchial tears are associated with crushing injuries suffered in high-speed motor vehicle accidents. Their true incidence is unknown because patients often die (from the disruption or from associated injuries) before getting to the hospital. The overall mortality is estimated at 30 percent, but 90 percent of patients reaching the hospital alive can expect full recovery. Prompt recognition of the injury and early treatment greatly reduce morbidity and increase the chances of restoring normal pulmonary function.
Read more
Posted in Bronchus Avulsion | 10/01/2015
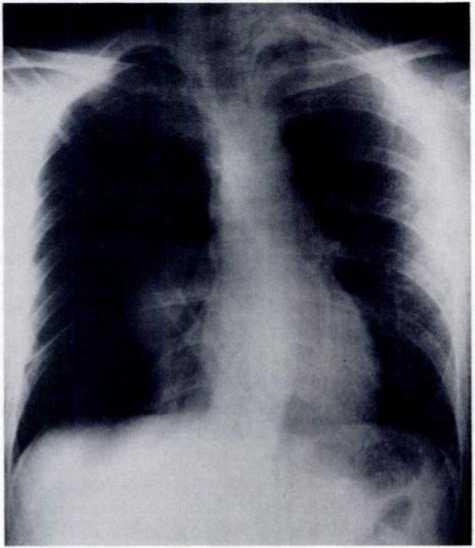
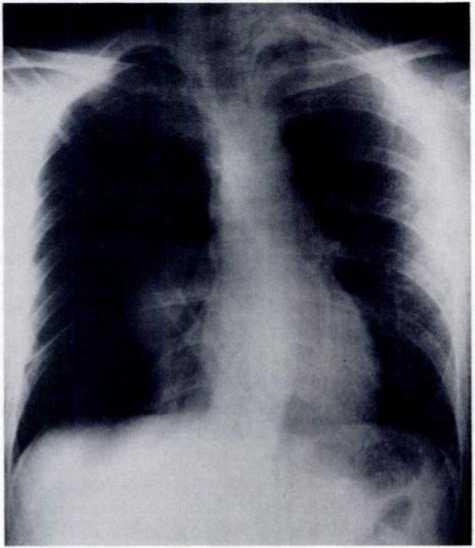
A 26-year-old man was the front seat passenger in a car involved in a head-on collision. He was brought to the emergency room of a local hospital, where initial evaluation showed a mild dyspnea and a deep, 4-cm, left-sided cervical laceration through which air was heard gushing out. A roentgenogram of the chest revealed a right-sided tension pneumothorax. A chest tube was inserted into the right pleural space and the patient transferred. Upon arrival, some 6 h after the accident, the patient was conscious and neither dyspneic nor unstable. Minimal subcutaneous emphysema was present over the left side of the neck, and large air leaks from both the chest tube and the cervical wound were noted. There were no associated injuries.
Read more
Posted in Airflow Obstruction | 09/01/2015
The above-mentioned studies demonstrate that the majority of nebulizers are less efficient than MDI at delivering bronchodilators, but that this lack of efficiency is more than compensated for by the striking excess of dose usually prescribed for the nebulizer (20-25 times the usual maintenance MDI dose). The results of the acute response study demonstrated no significant difference between metered-dose inhaler and nebulizer in the degree of bronchodilatation and improvement in 6-min walking distance. The findings of the outpatient study also demonstrated no difference between the two modes of delivery in FEVi, 6MWD, symptom scores, and extra beta-agonist use. The statistically significant improvement in VC after both treatment fortnights was small and unlikely to be clinically relevant. The 4-5 percent improvement in 6-min walking distance also reached statistical significance, but was not reflected in the patients’ perception of their exertional breathlessness.
Read more

Posted in Airflow Obstruction | 08/01/2015
Two recently published studies by Jenkins et al and Gunarwardena et al have demonstrated no clear advantage of nebulizers over metered-do$e inhalers. Jenkins et al studied patients with severe, poorly reversible airflow obstruction comparing equivalent doses of nebulized salbutamol and salbutamol administered by metered dose inhaler. There was no significant difference between the two delivery methods, but it is notable that this study was not strictly blinded in that the placebo nebulizing solution was saline rather than “dummy” salbutamol. The study by Gu-narwardena et al produced similar findings, but used only standard dose regimens of ipratropium bromide. http://acular-eye-drops.com/
Read more