Canadian HealthCare Mall: Results of Pulmonary Cell Populations from Patients with Carcinoma of the Lung
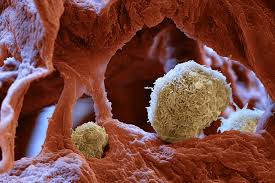 As shown in Table 1, interstitial cell populations obtained using the method described herein were predominantly composed of alveolar macrophages, with substantial percentages of both lymphocytes and neutrophils. No increase in the percentage of lymphocytes was seen in the interstitial cell populations contiguous to tumor. Cytotoxity was 1.3 percent or less at all ET ratios for interstitial cell populations from all patients with cancer. To confirm previous reports that the cell separation procedures used do not hinder the detection of natural killer activity, evaluation of apparently normal lung was also performed. Cytotoxic cell responses of 9.3±1.6 and 14.8±0.3 were demonstrated in interstitial cell preparations from the two control cell populations at the lowest ET ratio (50:1). At the ET ratio of 50:1, cytotoxicity of peripheral blood mononuclear cells from 15 nonsmoking normal control subjects studied in our laboratory was 28 ± 35 percent.
As shown in Table 1, interstitial cell populations obtained using the method described herein were predominantly composed of alveolar macrophages, with substantial percentages of both lymphocytes and neutrophils. No increase in the percentage of lymphocytes was seen in the interstitial cell populations contiguous to tumor. Cytotoxity was 1.3 percent or less at all ET ratios for interstitial cell populations from all patients with cancer. To confirm previous reports that the cell separation procedures used do not hinder the detection of natural killer activity, evaluation of apparently normal lung was also performed. Cytotoxic cell responses of 9.3±1.6 and 14.8±0.3 were demonstrated in interstitial cell preparations from the two control cell populations at the lowest ET ratio (50:1). At the ET ratio of 50:1, cytotoxicity of peripheral blood mononuclear cells from 15 nonsmoking normal control subjects studied in our laboratory was 28 ± 35 percent.
Discussion
We hypothesized that since natural killer cells may be active in host defense against malignant disease, increased levels of natural killer activity might be present in interstitial pulmonary cell populations contiguous to malignant pulmonary tumors. This hypothesis was supported by the fact that cells cytotoxic for tumor cell lines (including the K562 line used here) and autologous tumor cells have been grown from fragments of tissue from malignant pulmonary tumors. Over 20 percent of these cells had surface antigens associated with the natural killer phenotype. Another study suggested that low levels of natural killer activity were present in density-gradient-purified pulmonary cell preparations from the lungs of patients with a variety of malignant and nonmalignant tumors and that this activity could be enhanced by depletion of adherent cells. Unfortunately, comparisons of natural killer reponses from cancerous and noncancerous lung are difficult in that study, as the source of pulmonary tissues was not clearly identified, no undiseased lung was studied, and the smoking status of the patients was not noted. This latter point is of considerable importance, as natural killer activity of lymphocytes from smokers appears to be significantly lower than that of nonsmokers. Our data are in agreement with a preliminary report which also found natural killer activity to be lower in interstitial pulmonary cell populations of patients with primary lung cancer. That study and others, also demonstrated that natural killer activity is down regulated in human lung by alveolar macrophages. Lymphocyte populations isolated directly from pulmonary tumor substance also appear to have decreased natural killer activity as compared to peripheral blood lymphocytes with similar percentages of cells bearing the natural killer phenotype. The last news from Canadian Health and Care Mall are here chcm4you.com.
The lack of demonstrable natural killer activity in interstitial pulmonary cell preparations from patients with cancer could be influenced by a number of variables, including the following: (1) the smoking status of the patient, which could affect either the numbers or function of natural killer cells present; (2) the ratios of pulmonary alveolar macrophages to natural killer cells in the lung; (3) the activation state of the pulmonary alveolar macrophages so far as their ability to produce suppression of natural killer cell function; (4) tumor-related suppressor factors; and (5) the presence and activity of cell populations, including activated T-lymphocytes, with the ability to secrete lym-pholdnes known to regulate natural killer activity. In order to understand these variables, future studies will require isolation of homogeneous populations of lymphocytes from pulmonary specimens of patients carefully grouped for smoking and tumor-related variables. Dose-response studies of natural killer function using carefully characterized mononuclear cell populations from peripheral blood and lung are required to determine if the defect noted is systemic or “compartmentalized” to the lung. Such studies are important, as it is now possible to up regulate the cytotoxic cell activity in vivo with a variety of biologic response modifiers, and augmentation of this activity could have clinical importance. This would appear to be especially important in light of our observations here that levels of pulmonary natural killer activity are lower in lungs from patients with cancer than from healthy individuals.
Table 1—Interstitial Cell Populations from Patients with Lung Cancer and Control Patients
| Group | No. of Subjects | PulmonaryAlveolarMacrophages | Lymphocytes | PolymorphonuclearLeukocytes | Eosinophils | Basophils | EsterasePositiveCellst |
| Squamous cell carcinoma | 3 | 85 | 12 | 2.0 | 1.7 | 0.4 | 44 |
| ±1.9 | ±2.1 | ±1.7 | ±1.3 | ±0.4 | ±6.5 | ||
| Adenocarcinoma | 3 | 74 | 13 | 11 | 1.0 | 1.0 | 45 |
| ±2.8 | ±3.2 | ±1.3 | ±0.5 | ±1.0 | ±3.5 | ||
| Metastatic tumor | 3 | 62 | 18 | 14 | 6.0 | 0.8 | 50 |
| ±4.3 | ±2.7 | ±3.2 | ±2.9 | ±0.8 | ±8.2 | ||
| Controls | 2 | 66 | 28 | 13 | 5.0 | 4.0 | 33 |
| ±14 | ±1.0 | ±4.5 | ±1.5 | ±0.5 | ±19 |
Category: Carcinoma
Tags: alveolar macrophages, Carcinoma, pulmonary tissue