Psychobiological Aspects of Asthma and the Consequent Research Implications: THE INTERACTION OF MEDICAL
The Interaction of Medical, Psychologic, and Social Issues in Asthma and Their Effect on Levels of Individual Disability
Asthma and the anxiety disorders are separate autonomous medical conditions. The relatively common occurrence, however, of anxiety disorders in asthmatics and in patients with other forms of chronic respiratory disease has been well documented, as has the production of asthma attacks by “suggestion” and the association between mood and pulmonary function. More recently in a single case study, Hibbert and Pilsbury employed ambulatory Pco2 monitoring to show that hyperventilation preceded the exacerbation of asthma in an anxious patient. In this case teaching the patient to control his breathing after hyperventilation led to his being able to avoid attacks of asthma. Furthermore, in two partially selected populations of 40 mild and 25 severe asthmatics, 22 (34 percent) of these patients had anxiety disorders diagnosed using DSM-III criteria, with 11 patients having panic disorders, seven having posttraumatic stress disorders, and four having phobic disorders. This rate of anxiety disorders is considerably higher than the 2 to 5 percent point prevalence of anxiety disorders that is generally accepted to occur in the general population.
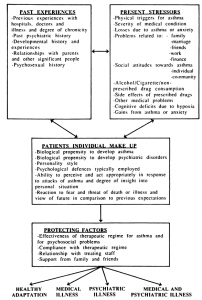
The interaction between medical and psychosocial factors leading to varying levels of individual adaptation to asthma can be understood by using the formulation presented in Figure 1. This diagrammatic representation of the dynamic interactions of medical and psychosocial issues in asthma allows an explanation and an understanding of the outcome in individual patients. It also emphasizes the interrelationships and connections between an individuals past and present experiences and his or her personality style as well as the biologic, psychologic, and social factors of importance in the production and perpetuation of asthmatic symptoms.
canadian antibiotics
There are a variety of indicators that suggest that biologic factors associated with psychiatric disorders may be of significance in asthma. It has been hypothesized that panic attacks may be secondary to increased sensitivity of medullary chemoreceptors; it is also noted that episodes of panic can be induced by C02 rebreathing, lactate acid infusion, or hyperventilation possibly through cerebral intraneu- ronal ischemia. It has been suggested that this may be occurring in patients with chronic airways obstruction where hyperventilation was hypothesized to be a physiologic response to a chronically elevated Pco2 level. Whether this occurs in patients with asthma, and this may only be when they are in respiratory failure, or whether it operates only in vulnerable asthmatics who have a specific neurophysiology or neuroanatomic abnormality, as discussed below, is open for conjecture, but it would seem to be plausible. Certainly it is known that normal subjects, for example, have a wide physiologic range of individual sensitivity to Pco2 levels, and one study has shown a relation between personality variables and ventilatory response to Pco2. It is possible that asthmatic patients who became anxious may be physiologically hypersensitive to raised, or to physiologically normal, levels of Pco2 with a resultant increased likelihood of hyperventilation. Evidence in support of a hypothesis of this kind is derived from the single case study of an anxious asthmatic reported by Hibbert and Pilsbury. Here voluntary hyperventilation predictably led to a fall in Pco2, but hyperventilation then continued involuntarily while further instructions about the study were given to the patient, following which asthma developed in conjunction with exercise.
FIGURE 1. Dynamic interaction of medical and psychosocial issues in asthma to explain outcome.
At an anatomic level the respiratory centers are positioned in the brain stem and are known to be connected via the hippocampal formation, a major reception area for all sensory modalities, to the para- hippocampal region. The parahippocampal region of the brain has been hypothesized to be anatomically different in patients with panic disorders, and these disorders are also known to be genetically linked, as is asthma. Reiman et al have used positron emission tomography to study patients who were susceptible to lactate-induced panic and noted, “an abnormal hemispheric assymmetry of parahippocampal blood flow, blood volume, and oxygen metabolism, as well as an abnormally high whole brain metabolism and an abnormal susceptibility to hyperventilation.” It is possible that either hyperventilation may lead to a parahippocampal abnormality and the production of continued panic attacks in asthmatics via a feedback loop or the parahippocampal abnormality may be present anyway, possibly as an inherited characteristic, and this may make patients more vulnerable to panic attacks if other psychosocial stresses occur. Furthermore, a recent discussion has postulated a physiologic link between depression and death from asthma via cholinergic pathways. It is possible that these pathways may also be involved in the etiology of anxiety disorders seen in asthmatics. Bass and Gardner have reviewed the many factors that influence breathing and have attempted to draw them all together in a diagrammatic representation of what they describe as a simplification of “the very complex feedback control system” in which they have incorporated both physical and psychologic factors. This control system took account of the large subjective component in the sensation of dyspnea as Bass and Gardner had noted the warning by Campbell and Howell that “a respiratory physiologist offering a unitary explanation for breathlessness should arouse the same suspicion as a tattooed archbishop offering a free ticket to heaven.”
buy levitra 20 mg
Category: Asthma
Tags: Asthma